
ÖYKÜ
45 yaşında kadın hasta, sağ yanak bölgesinde oluşan ekstra-oral fistül ve bu bölgede 4 aydır mevcut olan şişlikle kliniğimize başvurmuştur. Alınan anamnezde sistemik olarak herhangi bir hastalığı mevcut olmadığı öğrenilmiştir. Hastamız, parestezi oluşması ile beraber kliniğimize başvurma gereği duymuştur.
BULGULAR
Ekstraoral muayenede, fasiyal asimetri ve sağ prosesus kondilaris ile sağ submandibular alan arasında uzanım gösteren şişlik görülmüştür. Şişlik bölgesindeki deri çevre dokulara göre daha gergin olup palpasyonda hafif ağrı ile beraber fluktasyon ve ilgili bölgede lokal sıcaklık artışı hissedilmiştir. Lenfadenopati mevcut değildir.
Panoramik radyografide 48 numaralı diş bölgesinden başlayıp sağ ramus boyunca uzanım gösteren scallop ve hafif düzensiz sınırlı radyolusent lezyon izlenmiştir. Lezyon içerisinde, lezyonun diğer bölgelerinden daha radyolusent olan ve kortikal perforasyon ile uyumlu olabileceği düşünülen görüntü dikkat çekmiştir.
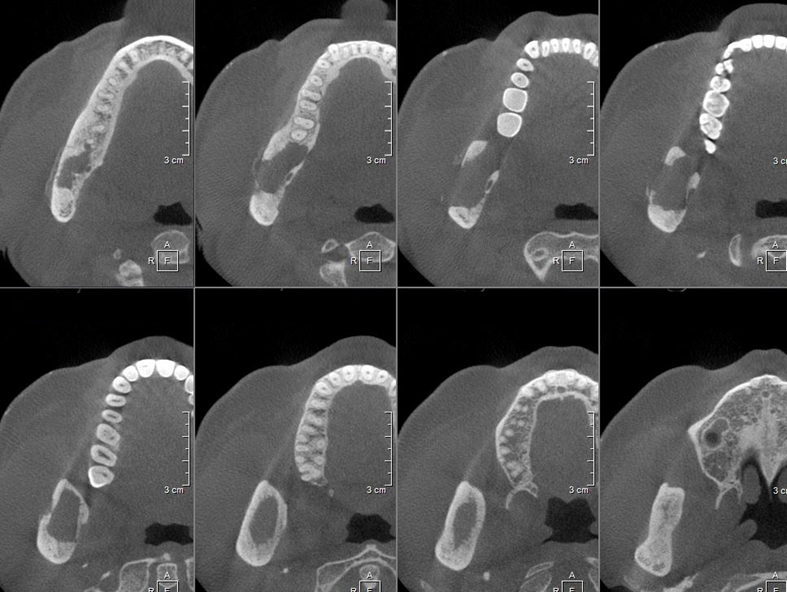
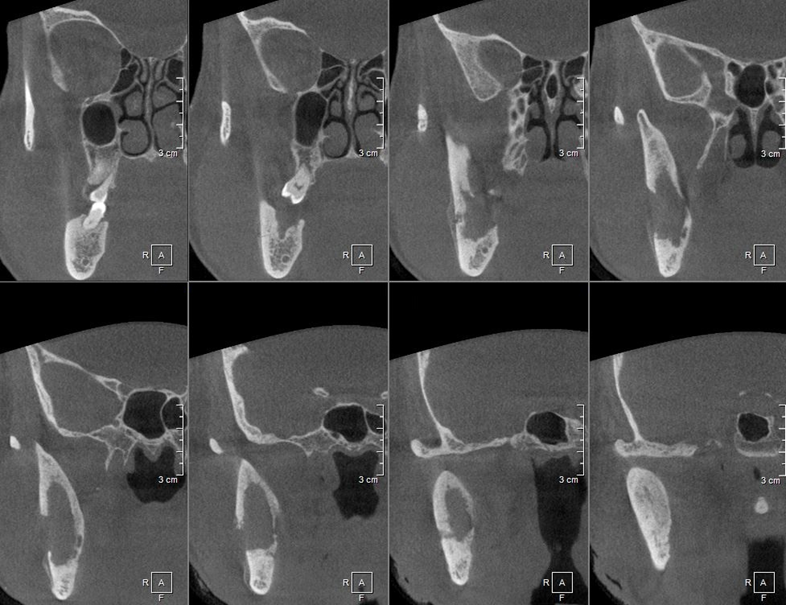
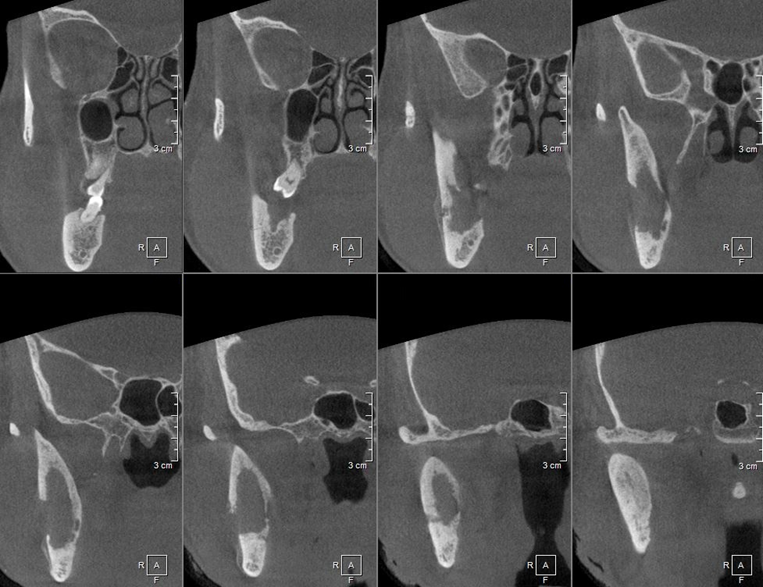
Sekonder enfekte bir odontojenik keratokist ön tanısı ile Konik Işınlı Bilgisayarlı Tomografi (KIBT) görüntüsü elde edilmiştir. KIBT kesitlerinde mandibula ramusunda uniloküler, düzenli sınırlı, hipodens ve mandibular kanalın üst sınırı ile temas halinde bir lezyon izlenmiştir. Lezyon bukkal ve lingual kortikal kemikte yıkıma neden olup bukkal bölgede, agresif lezyonlara eşlik eden Codman üçgeni tipte periosteal reaksiyon görülmüştür.
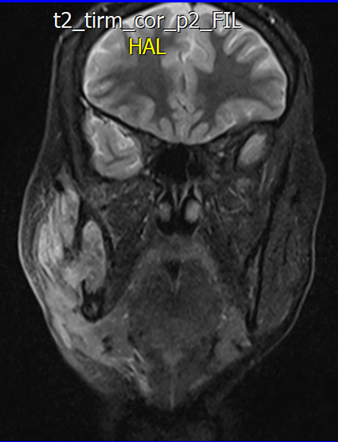
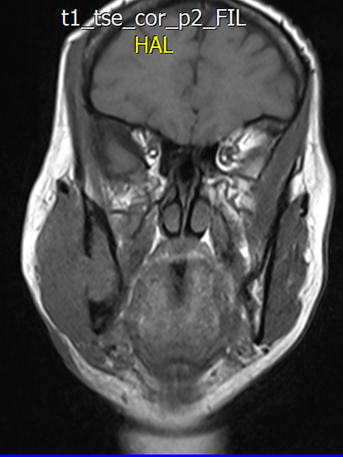
Koronal T2 Turbo Inversion Recovery Magnitude (TIRM) MRG görüntüsünde, mandibula ramusunun trabeküler aralığından bukkal bölgeye doğru kortikal yıkım ile uzanım gösteren lezyon ile ilgili diffüz ve artmış sinyal intensitesine sahip yumuşak doku alanları izlenmiştir.
TANI
İnsizyonel biyopsi sonucunda yapılan histopatolojik ve radyolojik değerlendirme sonucunda lezyon Primer İntraosseöz Karsinoma tanısı alıp radikal rezeksiyon ve boyun diseksiyonu yapılmıştır. 2018 yılından itibaren takipte olan hastamızda herhangi bir nüks ile karşılaşılmamıştır.
TARTIŞMA
Dünya Sağlık Örgütü 2017 sınıflamasına gören Primer İntraosseöz Karsinoma (PIOC) diğer karsinoma tipleri ile aynı kategoride bulunmayan santral bir çene karsinomudur. Odontojenik epitelden geliştiği bilinen PIOC’lar bazı olgulardan odontojenik kistlerin veya benign tümörlerin epitellerinden köken alabilmektedir. Primer odontojenik karsinoma olarak da bilinen PIOC’lar, ender tümörler olup 2011 yılına kadar yalnızca 116 olgu bildirilmiştir.
Genellikle mandibula posterior ve ramus bölgesinde lokalize olan bu lezyonlar için ayırıcı tanıda oral mukozadan gelişen skuamöz hücreli karsinomalar ve metastatik karsinomalar ekarte edilmelidir. Lokalizasyon, ayırıcı tanıda büyük öneme sahip olup mandibular kanalın inferiorundaki lezyonların metastaz, superiorunda bulunan lezyonların PIOC yönünde ön değerlendirilmesi gerekmektedir. Olgumuzdaki gibi kistlerden gelişen PIOC’lar mandibulada daha sık bildirilmiştir.
Çoğu PIOC asemptomatk olup tesadüfi olarak ortopantomograflarda tespit edilir. İleri olgularda maligniteleri işaret eden ekspansiyon, ağrı, ülserasyon, dişlerde mobilite, iyileşmeyen çekim soketleri, patolojik fraktür gibi non-spesifik bulgular izlenebilir PIOC’lar genellikle kök rezorpsiyonuna ve kortikal kemik yıkımına neden olan düzeniz sınırlı hipodens lezyonlar olmalarına karşın kistlerden gelişen PIOC’ların, olgumuzda olduğu gibi, düzenli sınırlı, multiloküler veya scallop yapıda olduğu rapor edilmiştir. Hastaların yaklaşık %40’ında metastaz mevcuttur. Kistlerden gelişen PIOC’lar en sık olarak sırasıyla radiküler/rezidüel kistlerden, dentigeröz kistlerden ve odontojenik keratokistlerden gelişmektedir.
Prognozu ile ilgili keskin ifadeler için gerekli olgu sayısı mevcut olmamakla birlikte 2001 itibariyle 5-yıllık sağkalım %52 olarak ifade edilmiştir. Bu yüzde kistlerden gelişen PIOC’lar için %40 olarak ayrıca belirtilmiştir. Tedavisinde radikal rezeksiyon, metastazı önlemek için boyun diseksiyonu önerilmiştir. Lezyonların %60’ında lokal rekürrens mevcut olup uzak metastaz sık görülmemektedir. PIOC’lar metastaz yaptıkları takdirde genellikle akciğer metastazı görülmektedir.
YAZAR
Dr. Gürkan Ünsal1,2
1Yakın Doğu Üniversitesi, Diş Hekimliği Fakültesi, Ağız, Diş ve Çene Radyolojisi Anabilim Dalı
2Yakın Doğu Üniversitesi, DESAM Enstitüsü, Tıpta Yapay Zeka Araştırma Grubu
GÖRÜNTÜLEME BULGULARI
Figür 1: Panoramik Radyografi

Figür 2: Aksiyal KIBT kesitleri
Figür 3: Koronal KIBT kesitleri
Figür 4: Sagittal KIBT kesitleri
Figür 5: Koronal MRG kesiti [T2 Turbo Inversion Recovery Magnitude (TIRM)]
Figür 6: Koronal MRG kesiti (T1 Turbo Spin Echo (TSE))
KAYNAKLAR
- Wright JM, Vered M. Update from the 4th edition of the World Health Organization classification of head and neck tumours: odontogenic and maxillofacial bone tumors. Head Neck Pathol. 2017;11(1):68–77.
- Eversole LR, Siar CH, van der Waal I. Primary intraosseous squamous cell carcinomas. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. p. 290–1.
- Ye P, Wei T, Gao Y, Zhang W, Peng X. Primary intraosseous squamous cell carcinoma arising from an odontogenic keratocyst: case series and literature review. Med Oral Patol Oral Cir Bucal. 2021;26(1): e49–55.
- Orhan, K. Ünsal, G. Applications of Ultrasonography in Maxillofacial/Intraoral Benign and Malignant Tumors. 2021.
